Achilles Pain When Running: Common Causes, Warning Signs, and How to Prevent Injury
Achilles pain when running is common. Learn causes, warning signs, prevention tips, and when to seek care from FAS The Woodlands.

Itchy, red, or peeling skin on your feet can be more than just an irritation; it could be a sign of a skin condition that requires different care. Athlete’s foot and foot eczema are two of the most common causes of foot irritation, yet they’re often confused with each other. While they may look similar at first glance, their causes, treatments, and even risks are very different.
Understanding how to tell them apart can save you from months of frustration and ensure you get the right treatment from the start.
Athlete’s foot (or tinea pedis) is a fungal infection that develops when dermatophyte fungi—microorganisms that thrive on keratin—invade the top layer of skin. These fungi love warm, damp environments, making feet (especially between the toes) the perfect host.
The infection is contagious and can spread through direct contact, shared towels, shoes, or contaminated surfaces like gym floors and locker rooms.

You’re more likely to develop athlete’s foot if you:
Although it’s uncomfortable, athlete’s foot can usually be managed effectively with antifungal treatment and proper foot hygiene.
Foot eczema is not an infection, it’s an inflammatory skin condition caused by a weakened or overreactive immune response that disrupts the skin barrier. When this barrier is compromised, moisture escapes and irritants enter, leading to dry, itchy, and inflamed skin.
Unlike athlete’s foot, eczema is not contagious. It often affects people with a history of allergies, asthma, or atopic dermatitis and can appear anywhere on the body, including the feet.

Eczema flares on the feet can be caused by:
Eczema can be chronic, with flare-ups that come and go. While it can’t be “cured,” it can be managed effectively through daily skincare, moisturizers, and prescribed topical treatments.
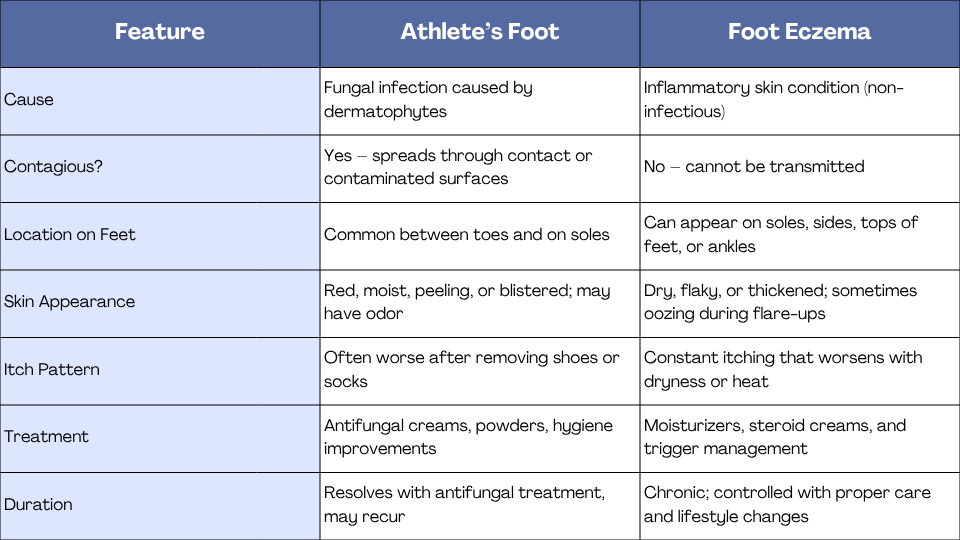
At first glance, both conditions can cause redness, peeling, and itching, which is why many people misdiagnose themselves. Treating eczema with antifungal creams won’t help, and using steroid creams on a fungal infection can actually make it worse.
Only a podiatrist or dermatologist can accurately determine the cause, often through a simple skin scraping or culture test to confirm if fungus is present.
A proper diagnosis ensures you’re not wasting time (and money) on the wrong treatment and helps prevent complications like secondary infections or skin damage.
Here are a few quick clues that can help:
Still unsure? It’s always best to let a podiatrist confirm the diagnosis rather than guessing based on appearance.
Treating Athlete’s Foot
If you’re prone to athlete’s foot, you may also want to read our guide on the best shoes for foot pain and how to choose the right footwear for comfort and support.
If your symptoms include peeling or pain, you may also benefit from our detailed guide on how to relieve pain from athlete’s foot, which covers overlapping care and prevention strategies.
Don’t wait for symptoms to worsen. Schedule a professional evaluation if you notice:
For more guidance, explore our educational post on when to see a podiatrist and the 10 signs you shouldn’t ignore.
Although athlete’s foot and foot eczema can look similar, their causes and treatments are entirely different. Athlete’s foot is a fungal infection that thrives in moisture and spreads easily; foot eczema is an inflammatory condition that results from skin barrier dysfunction.
If you’ve tried home remedies with little success, it’s time to see a podiatrist. A professional evaluation ensures accurate diagnosis, effective treatment, and relief that lasts.
At FAS The Woodlands, our foot and ankle specialists offer expert diagnosis and advanced treatment for all types of skin and nail conditions—from athlete’s foot and eczema to chronic dryness, nail fungus, and diabetic foot care.
📍 Serving The Woodlands, Huntsville, and Memorial City. Book your appointment today to restore healthy, comfortable feet.

Achilles pain when running is common. Learn causes, warning signs, prevention tips, and when to seek care from FAS The Woodlands.
.png)
Can bunions be corrected without surgery? Learn what natural treatments can relieve pain, what they cannot fix, and when professional bunion care is recommended.