Hammer Toes 101: What They Look Like, What Causes Them, and the Most Effective Treatment Options
Learn what hammer toes look like, what causes them, and the most effective treatment options, from early care to surgery, at FAS The Woodlands.
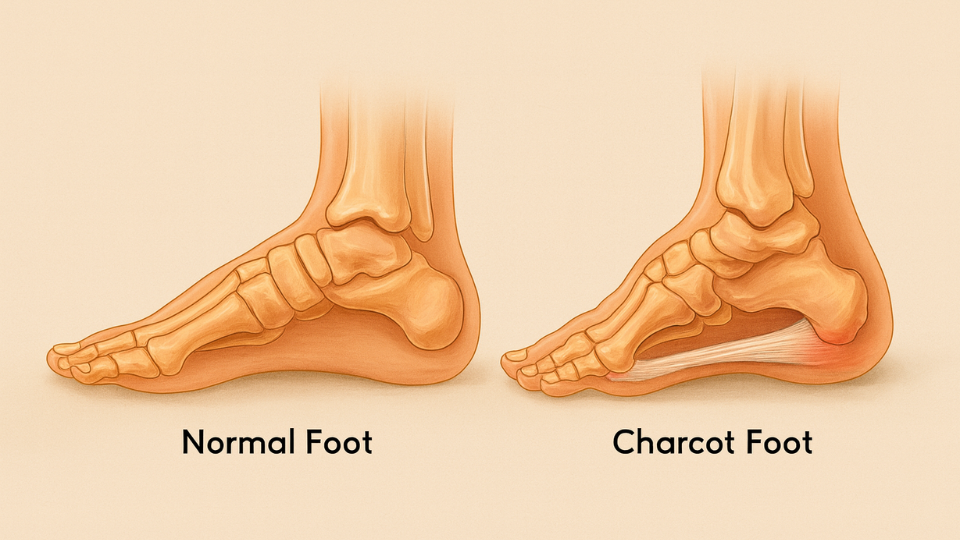
Charcot foot is one of the most serious and often misunderstood complications of diabetes. It involves progressive weakening and damage to the bones, joints, and soft tissues in the foot, often without significant pain in the early stages due to peripheral neuropathy. Because symptoms can be subtle at first, early diagnosis is critical to prevent fractures, deformities, and even amputation.
This guide will walk you through what Charcot foot is, why it develops, and the best approaches for effective Charcot foot management so you can protect your mobility and long-term foot health.
Charcot foot (also called Charcot arthropathy) is a condition where weakened bones in the foot fracture or dislocate easily, often without the person noticing due to nerve damage. Over time, this leads to changes in foot shape, arch collapse, and joint instability.
It’s most common in people with diabetic peripheral neuropathy. This condition makes it difficult to feel pain, heat, or pressure, allowing small injuries to go unnoticed and worsen over time. You can learn more about its causes, symptoms, and treatment options in our detailed guide on neuropathy in feet.
When left untreated, Charcot foot can progress quickly. Bones may shift out of place, and the foot can become deformed. These changes increase the risk of skin breakdown, ulcers, and severe infections.
The earlier Charcot foot is diagnosed and managed, the better the chances of preventing permanent damage.
Catching the condition early is critical to prevent serious damage. Unfortunately, many people miss the first signs because the changes can be subtle, especially if you have diabetes or peripheral neuropathy and can’t feel pain in your feet as well. Be alert for these early red flags:
Because Charcot foot often develops in people with peripheral neuropathy, recognizing nerve damage early is key to preventing severe complications. If you’re unsure whether you have neuropathy, watch for warning signs like tingling, numbness, or burning sensations in your feet. You can learn more about these symptoms in our guide on the 5 Signs of Peripheral Neuropathy.
If you notice even one of these symptoms, it’s important to get your foot evaluated by a podiatrist right away. The earlier treatment begins, the better your chances of avoiding irreversible deformity or loss of mobility.

One of the most important steps in Charcot foot management is taking pressure off the affected foot. This often involves:
This phase can last several months, allowing bones and joints to stabilize.
Once the active stage of Charcot foot has healed, custom orthotics can help prevent further damage. These are designed to accommodate any changes in foot shape, redistribute weight, and reduce pressure points.
If you want to learn more about whether custom orthotics or store-bought insoles are right for you, read our guide: Custom Orthotics vs. Over-the-Counter Insoles: Which Is Right for You?
Daily inspection of the feet is a must, especially if sensation is reduced or if you are living with diabetes, which significantly increases the risk of ulcers and slow-healing wounds. Look for:
Keeping the skin healthy helps avoid wounds that could lead to infection.
Follow-up visits with a podiatrist are critical in Charcot foot management. Regular imaging may be needed to ensure the bones remain stable, and adjustments to footwear or orthotics can be made as needed./;
If you or a loved one is living with Charcot foot, early and consistent care is key to preventing long-term problems. At Foot & Ankle Specialists (FAS) The Woodlands, our team provides comprehensive Charcot foot management plans tailored to your needs, from advanced offloading devices to custom orthotics and preventive care.
Don’t wait until symptoms worsen. Schedule an appointment with our team today and take the next step toward protecting your feet.

Learn what hammer toes look like, what causes them, and the most effective treatment options, from early care to surgery, at FAS The Woodlands.

Learn the common causes of a bump on the bottom of your foot, including nodules and hard lumps, plus symptoms to watch for and when to see a podiatrist at FAS The Woodlands.