Hammer Toes 101: What They Look Like, What Causes Them, and the Most Effective Treatment Options
Learn what hammer toes look like, what causes them, and the most effective treatment options, from early care to surgery, at FAS The Woodlands.
.png)
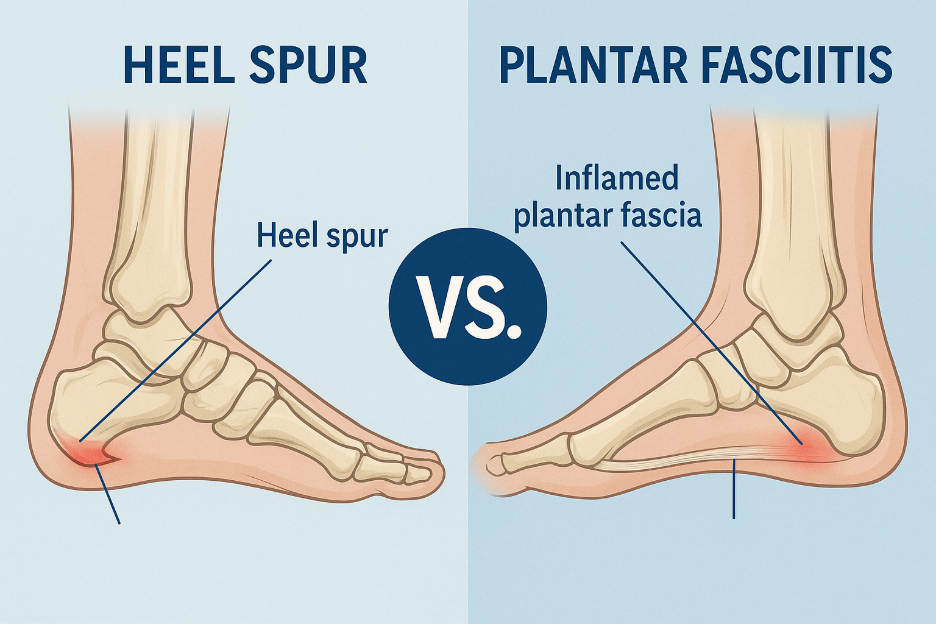
Heel pain is one of the most common complaints podiatrists hear from patients, and two conditions are often at the center of it: heel spurs and plantar fasciitis. These terms are sometimes used interchangeably, but they are not the same. Understanding the difference between a heel spur and plantar fasciitis is key to getting the right diagnosis and treatment plan.
In this article, we’ll break down what each condition is, how they differ, how they’re diagnosed, and what treatment options can bring lasting relief.
Plantar fasciitis is one of the leading causes of heel pain. It occurs when the plantar fascia, a thick band of tissue connecting your heel bone to your toes, becomes inflamed or strained.
Most cases are diagnosed through a physical exam and patient history. Imaging such as ultrasound or MRI may be used if symptoms don’t improve or another issue is suspected.
A heel spur is a bony growth (calcium deposit) that develops on the heel bone, often where the plantar fascia attaches. These spurs can look dramatic on X-rays, but the surprising truth is that many people have them without any pain at all.
A heel spur may contribute to discomfort if it aggravates the plantar fascia, but it is not always the primary cause of heel pain.
While the two conditions can exist together, they are distinct. Here’s how to tell them apart:
Because these conditions often overlap, treatment is usually similar. Most patients improve with conservative care and do not need surgery.
If symptoms don’t improve after several months of conservative treatment, your podiatrist may recommend:
If heel pain lasts more than a few weeks despite rest and home remedies, it’s important to see a podiatrist. A professional evaluation ensures you get the right diagnosis and treatment. Since heel spurs and plantar fasciitis can coexist, it takes expertise to determine which one is actually causing your pain.
Even after recovery, prevention is key to avoiding recurrence. Helpful strategies include:
The difference between a heel spur and plantar fasciitis lies in their origin: plantar fasciitis is a soft tissue problem, while a heel spur is a bony growth. While they may occur together, plantar fasciitis is usually the main cause of heel pain.
If you’re experiencing persistent heel pain, don’t wait for it to worsen. At FAS The Woodlands, our podiatrists specialize in accurate diagnosis and advanced treatment to get you back on your feet comfortably.
Take the first step toward pain-free living: Book an appointment today.

Learn what hammer toes look like, what causes them, and the most effective treatment options, from early care to surgery, at FAS The Woodlands.

Learn the common causes of a bump on the bottom of your foot, including nodules and hard lumps, plus symptoms to watch for and when to see a podiatrist at FAS The Woodlands.